The Silent Barrier to AI in Healthcare: Data Infrastructure
BlogsBy The BigRio Executive Team
And how CXOs can build the systems to power future-ready, compliant, and scalable transformation.
Executive Summary
Artificial Intelligence is poised to transform healthcare but only if it’s grounded in the right foundation. Despite growing investments in AI, most billion-dollar health systems are under-delivering on its promise. The core reason? A lack of AI-ready data infrastructure.
The future of AI in healthcare will not be determined by algorithms, but by the systems that enable them: governed, interoperable, privacy-resilient data environments that support continuous learning. Without these, even the most sophisticated AI models will fail to scale, suffer from clinical mistrust, and increase regulatory risk.
This article reframes the AI challenge from a model-centric problem to an infrastructure challenge. It outlines a blueprint for healthcare CxOs to design, fund, and govern an AI-ready data architecture, one that delivers not only compliance, but also clinical and financial ROI.
“Healthcare AI success won’t be driven by the smartest algorithm, but with the smartest infrastructure.”
Move from AI experimentation to AI orchestration
Across the boardroom, AI is being celebrated as the next frontier of innovation. Predictive diagnostics, automated charting, AI-driven decision support, it all sounds like the future. But in most health systems, these capabilities remain trapped in isolated pilots or innovation labs.
85% of healthcare AI initiatives fail to move beyond pilot stage, not due to model performance, but because of disjointed, low-quality, and siloed data. The gap is not vision, it’s execution. And the barrier to execution is infrastructure.
To operationalize AI at scale, healthcare organizations must invest in three infrastructure pillars
1. Governed & Interoperable Data
Healthcare organizations are drowning in data but that data exists across a multitude of incompatible systems: EHRs, lab information systems, imaging archives, wearables, and payer platforms. To make AI work at scale, these disparate sources must be connected through governed, interoperable infrastructure. Deploying FHIR-based APIs, integrating a federated data architecture, and establishing automated data quality pipelines allow organizations to harmonize and trust their data. The business impact is significant: reconciliation costs can drop by 40%, AI model accuracy improves, and regulatory risks tied to analytics are reduced. This foundation enables cross-functional data collaboration and supports advanced analytics and clinical decision-making across the enterprise.
2. Privacy-Resilient Data Access
Healthcare AI innovation is often slowed or completely blocked by the complex web of privacy regulations surrounding protected health information (PHI). These constraints create delays, elevate risk, and discourage experimentation. To navigate this, leading organizations are adopting privacy-resilient architectures that accelerate innovation while safeguarding patient data. By leveraging synthetic data to create de-identified yet statistically rich training environments, implementing federated learning across decentralized systems, and embedding differential privacy into model pipelines, organizations can maintain compliance without sacrificing agility. The payoff is significant: AI deployment cycles shrink by 50%, data breach risks are mitigated, and the organization is positioned as a privacy-first innovator in a trust-critical industry.
3. Continuous Learning & AI Resilience
“AI is not a one-time deployment. It’s a living system that must evolve with your data”
AI is not static, it’s a living system that must evolve with the health system it supports. Over time, as patient demographics shift, disease patterns change, and medical practices adapt, AI models trained on historical data can lose accuracy, reliability, and clinical trust. To prevent this degradation, leading organizations are implementing resilient infrastructures that ensure AI systems can adapt in real time. This includes establishing AI Ops pipelines for continuous monitoring, retraining, and auditing; embedding explainability tools like SHAP and LIME to provide transparency into model decisions; and incorporating human-in-the-loop workflows to ensure clinical oversight. These strategies not only increase physician confidence and adoption but also reduce costly downtime and improve compliance with traceable audit trails that stand up to regulatory scrutiny.
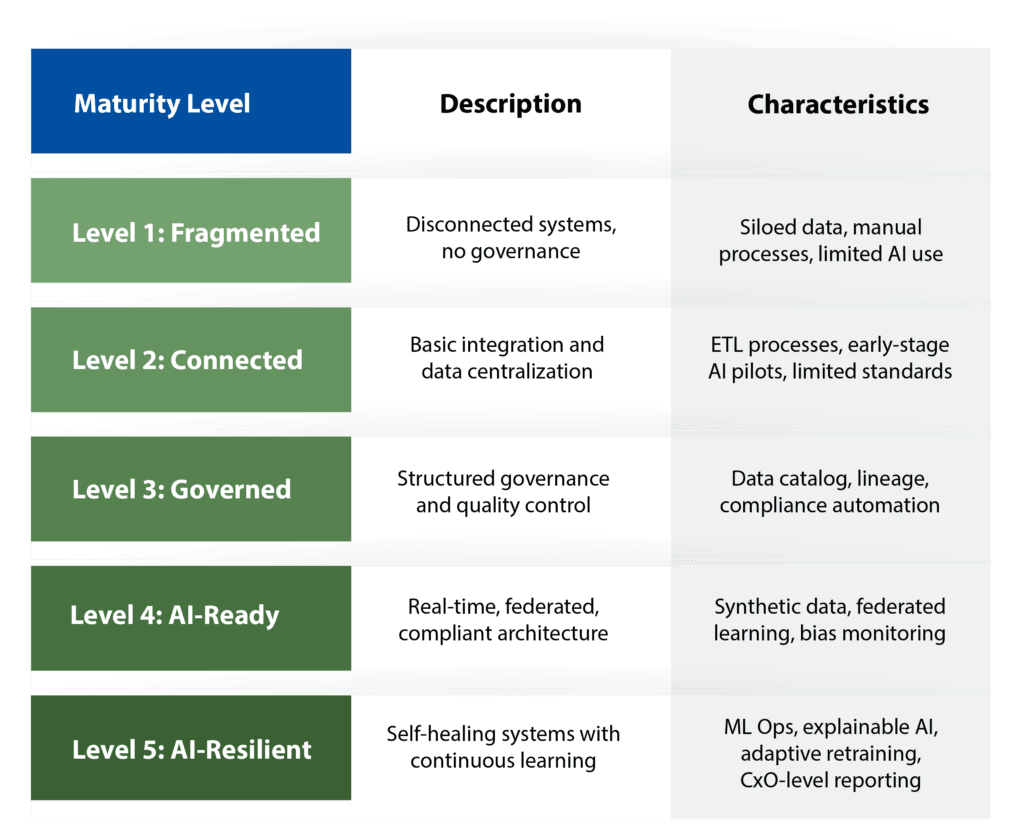
AI Infrastructure Maturity Model
Building an AI-powered healthcare enterprise is not a binary state, it’s a journey across maturity levels. The AI Infrastructure Maturity Model provides a framework for assessing where your organization stands today and what steps are needed to evolve. It spans from basic data fragmentation to fully orchestrated, self-improving systems capable of scaling AI securely, ethically, and effectively. This model enables CxOs to benchmark readiness, prioritize investments, and align AI ambitions with operational reality.
What Leading Health Systems Are Doing Right
Healthcare leaders are no longer treating AI as a research initiative, they’re operationalizing it through infrastructure-first strategies.
- Mayo Clinic has implemented a federated data architecture that enables AI research and clinical application across multiple facilities. This model ensures data stays within institutional boundaries while allowing secure, governed model training – effectively balancing innovation and compliance.
- Mount Sinai has leaned into synthetic data as a catalyst for experimentation. By developing statistically valid, privacy-safe datasets, they’ve accelerated the testing and validation of AI models while dramatically reducing the overhead and risk associated with using real patient records.
- Kaiser Permanente has established a dedicated AI governance board composed of clinical, legal, and technology leaders. This cross-functional oversight ensures all AI systems are auditable, explainable, and aligned with enterprise ethics and regulatory mandates.
These initiatives aren’t isolated success stories, they represent a repeatable blueprint for CxOs seeking to embed AI readiness into their core enterprise strategy. Each system has taken a proactive, infrastructure-first approach, aligning technical architecture with executive accountability to drive scalable outcomes.
Governance & ROI: Where CxOs Must Lead
Investing in infrastructure is not just a technical decision – it’s a strategic one. AI-ready data environments:
- Unlock revenue protection through smarter billing and fraud detection
- Enable value-based care through population-level insights
- Reduce legal exposure with compliant, auditable AI pipelines
CxOs should define clear KPIs to measure infrastructure ROI:
- % of AI models deployed beyond pilot stage
- % reduction in data integration and reconciliation time
- % of AI decisions traceable through XAI frameworks
Checklist: Is Your Organization AI-Ready?
If you’ve checked fewer than four, your infrastructure may be limiting – not enabling – AI at scale.
- Do we operate a federated, governed data architecture across all major data sources?
- Are we using FHIR-based interoperability standards for seamless data exchange?
- Have we deployed synthetic data environments for privacy-compliant AI training?
- Is there a formal AI governance board or framework overseeing lifecycle, compliance, and ethics?
- Are AI models continuously monitored and retrained for drift, bias, and relevance?
- Do we have explainability tools in place to trace and justify every AI-assisted clinical decision?
CxO Playbook: The 6–12 Month Strategy
For AI to deliver meaningful outcomes at scale, healthcare organizations must treat infrastructure as an enterprise-wide transformation and not a siloed IT initiative. This playbook serves as a pragmatic guide for CxOs to operationalize AI readiness within 6 to 12 months. It focuses on aligning clinical, technical, and compliance teams to establish foundational capabilities, pilot safely, and build momentum for long-term scalability.
- Form an AI Infrastructure Task Force across IT, clinical, and legal
- Audit current data readiness using the maturity model
- Identify a high-impact AI use case (e.g., readmission prediction, sepsis detection)
- Deploy a synthetic data sandbox to test privacy-resilient training
- Implement federated learning in a pilot clinical domain
- Launch governance protocols for bias, drift, and explainability
Conclusion: AI Won’t Transform Healthcare. Infrastructure Will.
AI alone will not fix healthcare. Algorithms can’t drive change unless they are part of a broader infrastructure ecosystem that is secure, scalable, and aligned with clinical workflows.
The future belongs to organizations that treat data infrastructure as a strategic asset, not an IT function. Healthcare CxOs who invest today in AI-ready infrastructure will not only scale transformation, but shape the next era of care delivery – safer, faster, and smarter.
Remember, AI is not the future of healthcare. AI-readiness is. The organizations that build for scale, privacy, and resilience today will define tomorrow’s standard of care.