BigRio’s technical approach to data interoperability and integration in digital applications
Abstract
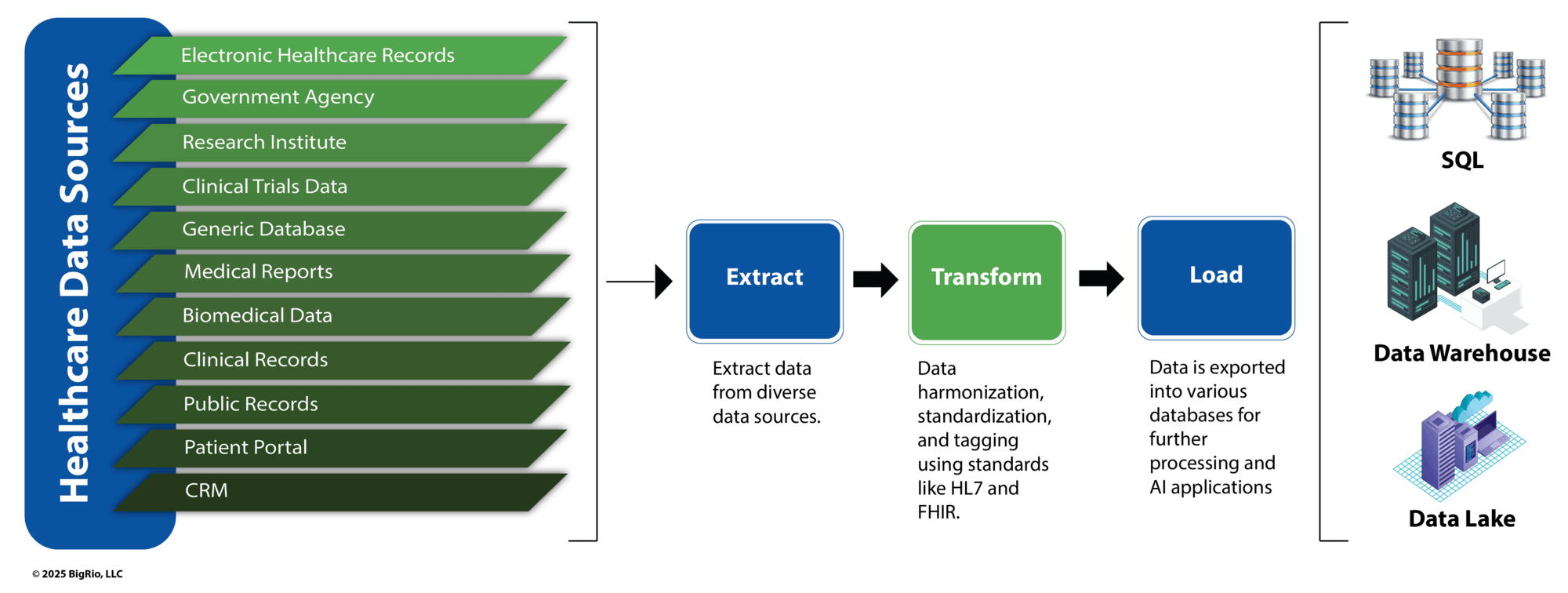
Data integration in healthcare remains a formidable challenge, as disparate systems and silos of information hinder seamless communication and collaboration across the industry. Electronic Health Records (EHRs), while critical to healthcare operations, often lack standardization, resulting in fragmented data and inefficient workflows. Extract, Transform, and Load (ETL) processes add to the complexity, as data from varied sources must first be cleansed, transformed, and standardized before it can be meaningfully integrated. These ETL challenges often create bottlenecks, further delaying the goal of interoperability.
Interoperability—the ability of systems to exchange and utilize data effectively—is central to overcoming these barriers. By leveraging industry standards such as HL7, FHIR, and CDA, along with advanced integration approaches like APIs and middleware platforms, healthcare organizations can enable cohesive data ecosystems. Further, cloud-based architectures, data lakes, and Master Data Management (MDM) support scalable and accurate data integration.
This white paper explores the critical concepts, standards, and technologies shaping healthcare data integration. It outlines the challenges of ETL processes, highlights the importance of interoperability, and discusses strategies to build robust architectures for seamless data exchange. Through these insights, digital health companies can overcome integration barriers, improve patient outcomes, and drive innovation in care delivery.
The Challenge of Data Integration in Healthcare
The healthcare industry has historically operated in silos, with different organizations and systems storing patient information in incompatible formats. These systems, especially Electronic Health Records (EHRs), have become the backbone of healthcare operations. However, they often rely on diverse standards, databases, and data models, making integration a complex and resource-intensive challenge. For example, patient demographics, diagnoses, and test results might be stored differently in EHRs, lab systems, and billing software, requiring significant effort to standardize and merge. Poorly implemented ETL workflows can result in data inconsistencies, delays, and errors, creating bottlenecks in the integration process.
For digital health companies developing remote monitoring, telemedicine, or health analytics applications, robust data integration is essential for offering value-added services. Without streamlined ETL pipelines and standardized integration, these companies risk inefficient workflows, incomplete patient records, and fragmented care delivery. Successfully navigating these challenges is a prerequisite to enabling interoperability and achieving comprehensive, data-driven healthcare solutions.
Figure 1: The ETL Pipeline in Healthcare
Importance of Interoperability
Interoperability is the ability of different information systems, devices, and applications to communicate, exchange, and use data effectively. In healthcare, this is not just about connecting EHRs but also integrating various other systems, such as laboratory information management systems (LIMS), medical billing systems, pharmacy systems, diagnostic equipment, and RPMs. Interoperability improves patient care by enabling healthcare professionals to access comprehensive, up-to-date patient information at the point of care.
Key Concepts in Data Integration
EHR Systems and Disparate Applications
Electronic Health Records (EHRs) are the backbone of healthcare IT systems, capturing comprehensive patient data such as medical history, diagnoses, medications, allergies, lab results, imaging reports, and treatment plans. However, significant variability in data models, communication protocols, and user interfaces often hinder their potential across different EHR vendors. This lack of standardization creates silos and complicates data interoperability.
In addition to EHRs, digital health companies rely on an expanding ecosystem of applications, including remote monitoring devices, telehealth platforms, wearable technologies, and advanced analytics engines. These applications often operate on diverse technological stacks, ranging from proprietary protocols to cloud-based architectures, further exacerbating integration challenges. The fragmented nature of these systems can lead to inconsistent data flow, duplicate records, and delayed access to critical patient information, ultimately impacting the quality of care.
Data Formats and Standards
Standardizing data formats is one of the key challenges in healthcare data integration. Some widely used healthcare standards include:
- HL7 (Health Level 7): A set of international standards for electronic data exchange in healthcare.
- FHIR (Fast Healthcare Interoperability Resources): FHIR is a modern standard developed by HL7, designed to enable simpler and faster data exchange between healthcare systems.
- CDA (Clinical Document Architecture): CDA is a standard for representing clinical documents such as discharge summaries, progress notes, and radiology reports.
Digital health companies must support and map these standards to the relevant systems for effective integration.
Integration Patterns
There are several integration patterns that digital health companies may use, depending on their needs:
- Point-to-Point Integration: Direct connections between applications. It is simple but can become challenging to maintain at scale.
- Hub-and-Spoke Model: Centralized integration via a middleware system that connects multiple systems.
- Service-Oriented Architecture (SOA): Decomposing an integration into microservices that communicate over a network enables better scalability and flexibility.
Each pattern has its advantages and challenges, and the choice will depend on factors such as scalability, real-time data needs, and the diversity of systems involved.
Integration Approaches Previously Followed in BigRio Client Engagements
Application Programming Interfaces (APIs)
APIs are a popular approach for system integration, enabling disparate systems to communicate over well-defined interfaces. Modern healthcare APIs often use RESTful services, making them easy to integrate with web and mobile applications. APIs allow flexibility and agility in adding or removing systems from the integration ecosystem.
FHIR APIs provide a lightweight, standards-based way to access and exchange patient data for EHR integration. For example, a digital health company developing a new remote monitoring app could use an EHR API to pull real-time patient data or send new readings from an RPM directly into a patient’s record.
HL7, FHIR, and CDA Standards
FHIR (Fast Healthcare Interoperability Resources) is important for modern digital health applications. Its modular approach breaks down healthcare data into small, reusable “resources” such as patients, medications, and observations, which can be easily shared across applications. FHIR APIs allow for better interoperability than traditional HL7 interfaces, as they are designed to be simpler and faster to implement.
- HL7: Traditional but widely adopted in legacy systems.
- FHIR: Newer, flexible, and designed for modern web-based apps.
- CDA: Useful for exchanging clinical documents but less granular than FHIR.
For integration, digital health companies must ensure they support the relevant standards for the systems they are working with.
Middleware and Integration Platforms
Middleware platforms such as InterSystems, Rhapsody, Mirth Connect, eiPlatform, Redox, and Cloverleaf are used to centralize integration tasks and manage system data flows. These platforms offer pre-built connectors, data transformation tools, and orchestration capabilities, simplifying the integration process.
Building a Robust Data Integration Architecture in the BigRio Way
Centralized vs. Decentralized Integration Models
- Centralized Integration: A single integration hub or enterprise service bus (ESB) acts as a central point where all systems connect. This model is efficient for organizations with many connected systems but can become a bottleneck if not designed correctly.
- Decentralized Integration: Distributed integration components, where systems are directly connected in a mesh network. This approach can be more flexible but requires careful management of data flows and error handling.
Data Lake, Lakehouse, and Cloud Integration
Cloud platforms such as AWS, Azure, and Google Cloud provide scalable environments for data integration. Cloud-based integration allows digital health companies to build data lakes that store large volumes of raw healthcare data, from EHRs to RPMs. This data can then be processed, analyzed, and shared across applications.
A data lake can also help integrate historical data, enabling more sophisticated analytics and predictive models. This integration is critical for improving patient outcomes through insights from aggregated data stored in platforms such as Snowflake and Databricks.
Master Data Management (MDM)
MDM is essential for ensuring that a single, accurate version of patient data is maintained across multiple systems. In healthcare, where data may exist in multiple systems (e.g., EHRs, pharmacies, laboratories), MDM ensures there is no inconsistency or duplication of data, which could otherwise lead to errors in patient care.
Conclusion
Data integration is the cornerstone of digital health innovation, serving as the foundation for unlocking the potential of advanced technologies like artificial intelligence and predictive analytics. While the healthcare industry has made significant strides in digitization, challenges such as disparate data sources, siloed systems, and complex ETL processes continue to impede progress toward interoperability. These barriers delay the realization of seamless data exchange and compromise the quality and efficiency of care delivery.
By adopting standardized frameworks such as HL7, FHIR, and CDA, alongside robust integration strategies like middleware platforms, APIs, and cloud-based architectures, digital health companies can transform fragmented healthcare data into unified ecosystems. These integrated solutions enable more accurate, timely, and comprehensive patient information, empowering clinicians and organizations to deliver better outcomes.
Moreover, investing in scalable data lakes, Master Data Management (MDM), and advanced ETL workflows lays the groundwork for future-ready healthcare systems capable of supporting AI-driven insights and value-based care models. In doing so, digital health companies can address current challenges and position themselves as leaders in the evolving healthcare landscape.
Ultimately, the path to overcoming data integration challenges is not merely a technical endeavor but a commitment to fostering innovation, improving patient care, and driving systemic transformation in healthcare. The industry can achieve the goal of truly interoperable, data-driven healthcare for all through strategic data integration efforts.